Abstract
This article reviews and updates a previously published study:
Ilie, Petre Cristian, Simina Stefanescu, and Lee Smith. “The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality.” Aging Clinical and Experimental Research (15 April 2020): 1. [7] PDF Link | Webpage Link
Ilie et al. found that “mean levels of vitamin D in various countries” were associated with “cases and mortality caused by COVID-19.” For nations with low vitamin D levels in the general population, cases per million persons and deaths per million persons were both significantly higher than for nations with higher levels of vitamin D. The level of vitamin D needed for the lower case and mortality rates was at the low end of the normal range.
The data used in the Ilie study for cases per million and deaths per million was from April 8th, 2020. This article compares that data to more recent data from Sept. 25th, 2020. The original findings of Ilie et al. are reviewed, and are compared to the more recent data. In addition, the Ilie study is examined with a new approach, that of combining the data from several nations, based on vitamin D levels, just as one would do for a set of patients.
Results
The conclusions of the Ilie study are upheld by this new evaluation of the April 8th data. Then the later data, from Sept. 25th, provides the same results, more clearly as more cases and deaths are available in the later data. Low vitamin D levels, on a national scale, are associated with higher rates of infection and death from Covid-19. In addition, higher vitamin D levels, at only the low end of the normal range, are associated with lower national case and mortality rates.
Introduction
Two questions are considered by this article. The first is whether the conclusions of the Ilie study, using data from April 8th, 2020, are confirmed by grouping the nations by range of vitamin D levels. The second is whether data from Sept. 25th, 2020, which includes 5.5 additional months of data (as well as earlier data), still supports an association between vitamin D levels and Covid-19 case and mortality rates at a national level.
The ilie study conclusions are summed up by the following two charts taken from the study: one for cases/million and one for deaths/million.
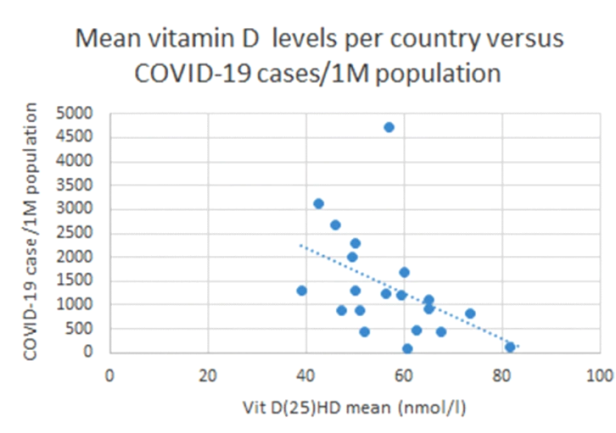

There is one data point above for each nation. The line in each chart shows the trend toward improvement with higher vitamin D levels. But what would the result be if we group the 20 European nations in the study by vitamin D level? Let’s group the nations by the nation average of vitamin D level.
Low - vitamin D below 50 nmol/l, which is below 20 ng/ml
Moderate - vitamin D from 50 to below 65 nmol/l, which is from 20 to below 26 ng/ml
Normal - vitamin D at 65 nmol/l or higher, which is at 26 ng/ml or higher
There are a few reasons for this categorization. First, a vitamin D level below 50 is a common definition of vitamin D deficiency. Second, vitamin D insufficiency is so common, there was literally only one nation (Slovakia) with a population-wide average vitamin D level in the normal range of 75 nmol/l and over (30 ng/ml and over). So the cut-off for the higher vitamin D level was chosen as 65 or higher instead of 75. This also made the three groups closer in the number of nations in each group. Even so, there were 10 nations in the middle group, as compared to 5 nations in each of the other two groups.
Here are the nations in each group:
Low Vitamin D: Portugal, Spain, Switzerland, UK, Belgium
Moderate Vitamin D: Italy, Germany, Estonia, Turkey, Ireland, Iceland, Netherlands, France, Hungary, Czech Republic
Normal Vitamin D: Norway, Denmark, Finland, Sweden, Slovakia
Why do the Nordic nations have better vitamin D levels? Some nations in that region have vitamin D food fortification programs, whether voluntary or required by law, and other nations benefit due to international commerce. If your company makes a vitamin D fortified food in, say, Sweden, you would want to expand your marketplace to include nearby nations. So a food fortification program can spill over into other nations in the region. But it is not clear how Slovakia obtained higher levels of vitamin D than many other nations.
In the chart below, cases per million of the population are compared based on the above three levels of vitamin D in each nation:
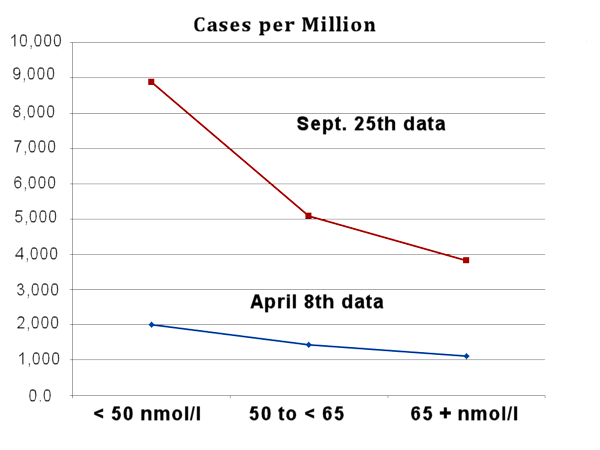
The lower line (blue diamonds) is from the Ilie study. But instead of a dot for each nation, the nations are grouped by vitamin D level. This is similar to the approach one would use with multiple patients.
Those nations (n=5) with national-average blood levels under 50 nmol/liter had higher cases/million than those (n=10) at 50 to <65 nmol/l. The difference is even larger when comparing the lowest to the highest group (5 nations in each group). In the earlier data (April 8), the infection rate is nearly double with the lowest compared to the highest levels of vitamin D. In the newer data (Sept 25), it is more than double. The newer data includes the entire time from the start of the pandemic to Sept. 25th.
In the newer data, the difference between the low and moderate vitamin D levels is greater than in the Ilie study. And notice the large increase in cases per million for nations with low vitamin D, as compared to only a moderate increase at the moderate vitamin D level and a lower increase in the normal vitamin D group. Nations with low vitamin D are continuing to do far worse in Covid-19 infection rates than those with vitamin D merely in the “insufficient but not deficient” level.
This fact highlights the ease with which vitamin D levels might be corrected. Raising the nations average level to the low end of the normal range, with many persons still at a level called “insufficient” would nevertheless be immensely beneficial — if this association is causal. How can we determine if the association is causal? Let’s do a study. Let’s raise the vitamin D levels of the entire world population, as much as possible (target level will be low end of normal) and see if the pandemic goes away. We can do the statistical analysis later.
The same association is seen in the next chart.
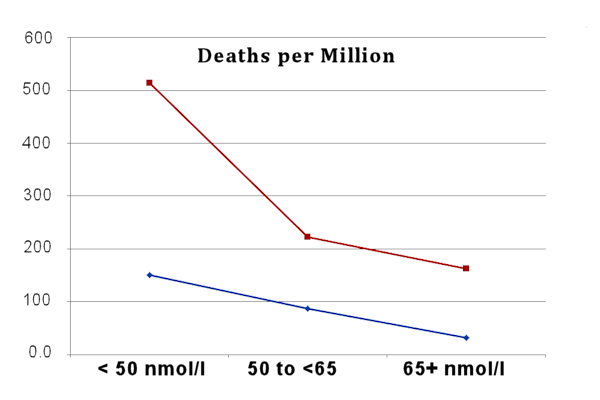
Deaths per million, in each of three groups, is associated with vitamin D level. The levels are higher with low vitamin D AND there was a large increase in nations with low vitamin D levels.
The Chart above essentially shows the number of lives that were lost due to the absence of a vitamin D program. What is needed is three or perhaps four things:
1. vitamin D food fortification, especially in flour and commonly eaten junk foods
2. strong recommendation of vitamin D supplementation
3. public service announcements on obtaining vitamin D from sunshine
4. In addition, nations should consider mandatory vitamin D supplementation in schools, corporations, and especially where employees are constantly exposed to many persons: store clerks and cashiers, health care providers, police, fire department, military, etc.
How many lives could be saved? Even a modest underfunded partially successful vitamin D “supplementation or sunshine” program (“SOS”) could easily cut the death rate in half. Look at the death rate chart. The increase in deaths for the nations with the lowest vitamin D is more than twice that of even the nations that had only modestly better vitamin D levels.
A successful vitamin D SOS program could cut the infection rate in half, thereby cutting the death rate in half, due to the lower number of cases, and, in addition, another 50% reduction could be obtained by the effects of vitamin D reducing the severity of the disease course.
Having normal healthy blood levels of vitamin D reduces Covid-19 risks, including risk of infection [7, 8, 9, 11, 12, 14, 16, 23, 27], of having a severe case [1, 3, 4, 5, 15, 17, 20, 22, 24, 25, 26], of needing hospitalization, ICU care, and/or mechanical ventilation [2, 10, 14, 15, 21, 22, 24, 26], as well as the risk of dying from Covid-19 [4, 6, 7, 9, 12, 13, 17, 18, 19, 22, 24, 25, 28].
Extending the Data
Notice the line in the Deaths per Million chart above. If we continue that line down to zero, what vitamin D level gives us, not really zero, but the lowest possible number of deaths obtainable by vitamin D levels? The answer, seen in the chart below, is 45.9 ng/ml or 114.75 nmol/liter level of 25(OH)D. The ideal vitamin D level from the Kaufman study [27] was about 50 ng/ml. So we should try to have a vitamin D level that is in the high 40’s or low 50’s. That is the maximum for good effects on Covid-19 from Vitamin D.

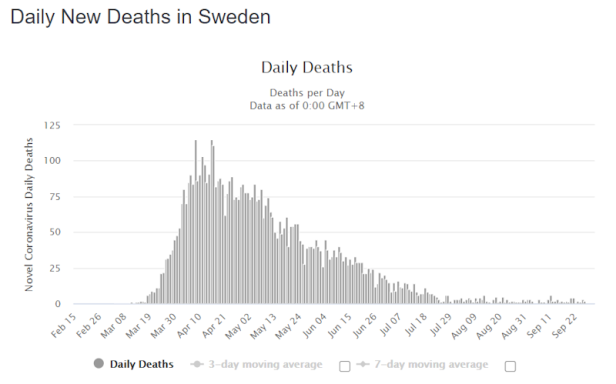
A Note About Sweden
One of the interesting points found in the Ilie study was that Sweden has one of the highest population-wide levels of vitamin D, and this resulted in low case and fatality rates. Out of the 20 European nations studied, Sweden had the second highest level of vitamin D. And now, months later, Sweden seems to have overcome Covid-19. Their case rate and death rates are very low. Their lives have almost returned to normal. But the Ilie study and this review point to vitamin D as a more probable cause of this benefit, rather than any hypothetical herd immunity. Too few cases of Covid-19 are found in Sweden to reach the usual level for Herd Immunity Threshold (HIT), which is 2/3rds.
Addendum
A reminder about the benefits of correcting vitamin D deficiency in any population: Additional benefits of vitamin D. Studies have shown that a high intake of vitamin D reduces risk of respiratory tract infections [101], stroke [102], multiple sclerosis [103], rheumatoid arthritis [104], type 2 diabetes [105], breast cancer [106], prostate cancer [107], colon cancer [108], and all-cause mortality [109].
Author: Ronald L. Conte Jr.
ENDNOTES
1. Alipio, Mark. “Vitamin D Supplementation Could Possibly Improve Clinical Outcomes of Patients Infected with Coronavirus-2019 (COVID-19).” SSRN 3571484 (9 April 2020).
Study Link
2. Lau, Frank H., et al. “Vitamin D insufficiency is prevalent in severe COVID-19.” medRxiv (28 April 2020).
Study Link
3. Daneshkhah, Ali, et al. “The Possible Role of Vitamin D in Suppressing Cytokine Storm and Associated Mortality in COVID-19 Patients.” medRxiv (2020).
Study Link
4. Davies, Gareth, Attila R. Garami, and Joanna C. Byers. “Evidence Supports a Causal Model for Vitamin D in COVID-19 Outcomes.” medRxiv (2020).
Study Link
5. De Smet, Dieter, et al. “Vitamin D deficiency as risk factor for severe COVID-19: a convergence of two pandemics.” medRxiv (2020).
Study Link
6. Raharusun, Prabowo, et al. “Patterns of COVID-19 Mortality and Vitamin D: An Indonesian Study.” (2020).
PDF file
7. Ilie, Petre Cristian, Simina Stefanescu, and Lee Smith. “The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality.” Aging Clinical and Experimental Research (2020): 1.
Study Link
8. D’Avolio, Antonio, et al. “25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2.” Nutrients 12.5 (2020): 1359.
Study Link
9. Laird, E., et al. “Vitamin D and Inflammation: Potential Implications for Severity of Covid-19.” Ir Med J; Vol 113; No. 5; P81: 2020.
PDF file
10. Faul, J.L., et al. “Vitamin D Deficiency and ARDS after SARS-CoV-2 Infection.” Ir Med J; Vol 113; No. 5; P84: 2020.
PDF file
11. Meltzer, David O., et al. “Association of Vitamin D Deficiency and Treatment with COVID-19 Incidence.” medRxiv (2020).
Study Link
12. Li, Yajia, et al. “Sunlight and vitamin D in the prevention of coronavirus disease (COVID-19) infection and mortality in the United States.” (2020).
PDF file
13. Pugach, Isaac Z. and Pugach, Sofya “Strong Correlation Between Prevalence of Severe Vitamin D Deficiency and Population Mortality Rate from COVID-19 in Europe.” medRxiv (2020).
Study Link
14. Merzon, Eugene, et al. “Low plasma 25(OH) vitamin D3 level is associated with increased risk of COVID-19 infection: an Israeli population-based study.” medRxiv (2020). — Low vitamin D increased risk (adjusted OR) of infection with Covid-19 by 45% and of hospitalization for Covid by 95%.
Study Link
15. Panagiotou, Grigorios et al., “Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity: results of a local audit of practice.” medRxiv (2020). Conclusion: “we found that patients requiring ITU admission [in the ICU] were more frequently vitamin D deficient than those managed on medical wards [on the floor], despite being significantly younger.”
PDF file Link
16. Chang, Timothy S., et al. “Prior diagnoses and medications as risk factors for COVID-19 in a Los Angeles Health System.” medRxiv (2020).
Study Link
~ Risk factors included vitamin D deficiency, which increased risk of COVID-19 diagnosis by 80% (OR 1.8 [1.4-2.2], p=5.7 x 10-6).
17. Maghbooli, Zhila, et al. “Vitamin D Sufficiency Reduced Risk for Morbidity and Mortality in COVID-19 Patients.” Available at SSRN 3616008 (2020).
Study Link
~ Vitamin D sufficiency reduced clinical severity and inpatient mortality.
18. Panarese and Shahini, “Letter: Covid-19 and Vitamin D” Alimentary Pharmacology and Therapeutics, April 12, 2020.
Link to Letter
~ Covid-19 mortality increases with increasing latitude (by nation), and vitamin D blood levels decrease with increasing latitude. The authors propose that low levels of vitamin D increase Covid-19 mortality.
19. Carpagnano, Giovanna Elisiana, et al. “Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19.” Journal of Endocrinological Investigation (2020): 1-7. Study Link
~ “A survival analysis highlighted that, after 10 days of hospitalization, severe vitamin D deficiency patients had a 50% mortality probability, while those with vitamin D = 10 ng/mL had a 5% mortality risk (p = 0.019).”
20. Mardani, R., et al. “Association of vitamin D with the modulation of the disease severity in COVID-19.” Virus Research (2020): 198148. Study Link
21. Castillo, Marta Entrenas, et al. “Effect of Calcifediol Treatment and best Available Therapy versus best Available Therapy on Intensive Care Unit Admission and Mortality Among Patients Hospitalized for COVID-19: A Pilot Randomized Clinical study.” The Journal of Steroid Biochemistry and Molecular Biology (2020): 105751. Study Link
** This was a peer-reviewed randomized placebo-controlled trial (RCT). It’s sufficient. See the Chris Masterjohn, Ph.D. commentary here.
22. Radujkovic, et al. “Vitamin D Deficiency and Outcome of COVID-19 Patients.” Nutrients 2020, 12(9), 2757; Study Link
— “The present study demonstrates an association between VitD deficiency and severity of COVID-19.
VitD-deficient patients had a higher hospitalization rate and required more (intensive) oxygen therapy
and IMV. In our patients, when adjusted for age, gender, and comorbidities, VitD deficiency was
associated with a 6-fold higher hazard of severe course of disease and a ~15-fold higher risk of death.”
23. Israel, Ariel, et al. “The link between vitamin D deficiency and Covid-19 in a large population.” MedRxiv 9/7/2020. Study Link
24. Jae Hyoung Im, et al. “Nutritional status of patients with coronavirus disease 2019 (COVID-19).”
International Journal of Infectious Diseases. August 7, 2020. PDF Link
25. Gennari L, et al “Vitamin D deficiency is independently associated with COVID-19 severity and mortality” ASBMR 2020; Abstract 1023. Study Link
26. Baktash, Vadir, et al. “Vitamin D status and outcomes for hospitalised older patients with COVID-19.” Postgraduate Medical Journal (2020). Study Link
— “The main findings of our study suggest that older patients with lower serum concentrations of 25(OH)D, when compared with aged-matched vitamin D-replete patients, may demonstrate worse outcomes from COVID-19. Markers of cytokine release syndrome were raised in these patients and they were more likely to become hypoxic and require ventilatory support in HDU.” [HDU is high dependency unit]
27. Kaufman HW, et al. “SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels.” (2020) PLoS ONE 15(9): e0239252. Study Link
— Optimum vitamin D blood level for reducing Covid-19 infection was found to be in the 50’s (ng/ml). This is the first study to show that 25(OH)D at levels above 30 have additional benefits.
28. Brenner, Hermann, Bernd Holleczek, and Ben Schöttker. “Vitamin D Insufficiency and Deficiency and Mortality from Respiratory Diseases in a Cohort of Older Adults: Potential for Limiting the Death Toll during and beyond the COVID-19 Pandemic?.” Nutrients 12.8 (2020): 2488.
— “Compared to those with sufficient vitamin D status, participants with vitamin D insufficiency and deficiency had strongly increased respiratory mortality, with adjusted hazard ratios (95% confidence intervals) of 2.1 (1.3–3.2) and 3.0 (1.8–5.2) overall, 4.3 (1.3–14.4) and 8.5 (2.4–30.1) among women, and 1.9 (1.1–3.2) and 2.3 (1.1–4.4) among men. Overall, 41% (95% confidence interval: 20–58%) of respiratory disease mortality was statistically attributable to vitamin D insufficiency or deficiency. Vitamin D insufficiency and deficiency are common and account for a large proportion of respiratory disease mortality in older adults, supporting the hypothesis that vitamin D3 supplementation could be helpful to limit the burden of the COVID-19 pandemic, particularly among women.”
Vitamin D and Other Diseases
101. Martineau, Adrian R., et al. “Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data.” bmj 356 (2017).
Study Link
— Recommend daily or weekly dose, but not bolus dosing.
102. Marniemi et al., Dietary and serum vitamins and minerals as predictors of myocardial infarction and stroke in elderly subjects; Nutrition, Metabolism & Cardiovascular Diseases. Volume 15, Issue 3 , Pages 188-197, June 2005. Study Link
103. Munger et al., Vitamin D intake and incidence of multiple sclerosis; Neurology. January 13, 2004 vol. 62 no. 1, p. 60-65. Study Link
104. Merlino et al., Vitamin D intake is inversely associated with rheumatoid arthritis: Results from the Iowa Women’s Health Study; Arthritis & Rheumatism. Volume 50, Issue 1, pages 72-77, January 2004. Study Link
105. Pittas et al., Vitamin D and Calcium Intake in Relation to Type 2 Diabetes in Women; Diabetes Care. March 2006 vol. 29 no. 3 650-656. Study Link
106. Garland et al., Vitamin D and prevention of breast cancer: Pooled analysis; The Journal of Steroid Biochemistry and Molecular Biology, Volume 103, Issues 3-5, March 2007, Pages 708-711; Study Link
107. Garland et al., The Role of Vitamin D in Cancer Prevention; American Journal of Public Health. 2006 February; 96(2): 252-261. Study Link
108. Gorham et al., Optimal Vitamin D Status for Colorectal Cancer Prevention: A Quantitative Meta-Analysis; American Journal of Preventive Medicine. Volume 32, Issue 3 , Pages 210-216, March 2007; Study Link
109. Antonio, Leen, et al. “Free 25-hydroxyvitamin D, but not free 1.25-dihydroxyvitamin D, predicts all-cause mortality in ageing men.” 22nd European Congress of Endocrinology. Vol. 70. BioScientifica, 2020.