Previously, we discussed six studies showing that higher vitamin D blood levels improved outcomes for Covid-19 patients, reducing the severity of the disease and reducing case fatality rate. These next studies add further information.
7. Ilie
The article is “The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality,” by Petre Cristian Ilie, Simina Stefanescu, and Lee Smith, published in “Aging Clinical and Experimental Research”. The study authors compared average vitamin D blood levels in European nations and compared this to the number of Covid-19 cases per 1 million of the population, and to the mortality per 1 million as well.
“We have identified a potential crude association between the mean vitamin D levels in various European countries with COVID-19 cases/1M and COVID-19 mortality.”
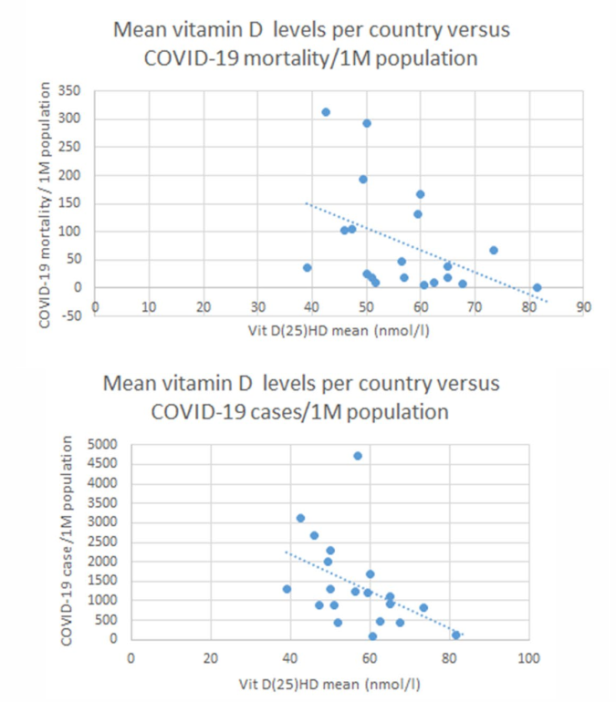
Notice that both the number of Covid-19 cases per million of the population and the mortality per million become quite low in the 60 to 80 nmol/l range (24 to 32 ng/ml). The benefit in that range is strong, yet the level of vitamin D is modest. Another study [1] used 30 or higher ng/ml (75 nmol/l) as the range for “normal” levels of vitamin D. So both studies agree that you don’t need a very high vitamin D level to obtain a substantial benefit against Covid-19.
A weakness of the Ilie study is that some nations may have relatively good vitamin D levels in most of the population. But the elderly, who are seldom outdoors, and who have reduced ability to make vitamin D from sunlight striking the skin, may have very low levels. So the nationwide average may be misleading. Most of the deaths from Covid-19 have been in the elderly.
A revision of the Ilie study should be done in which the vitamin D level in the elderly is compared to the case rate and mortality rate in that same population. So an elderly-specific version of the study might be more revealing, since that is where Covid-19 finds most of its victims.
8. D’Avolio
This study, by D’Avolio and seven other researchers, states its conclusion in its title: “25-Hydroxyvitamin D Concentrations Are Lower in Patients with Positive PCR for SARS-CoV-2” [13]. There is a clear correlation between lower blood levels of vitamin D — 25-Hydroxyvitamin D is the active form of the vitamin in the blood — and the likelihood of testing positive for Covid-19. This conclusion differs from the conclusions of the previous studies. Here, the authors are proposing that vitamin D reduces the risk of contracting Covid-19, rather than the risk of a severe case or the risk of death. We already know that vitamin D reduces the risk of contracting upper respiratory tract infections. So it is plausible that vitamin D could also affect the risk of contracting Covid-19.
“we retrospectively investigated the 25-hydroxyvitamin D (25(OH)D) concentrations in plasma obtained from a cohort of patients from Switzerland. In this cohort, significantly lower 25(OH)D levels (p = 0.004) were found in PCR-positive for SARS-CoV-2 (median value 11.1 ng/mL) patients compared with negative patients (24.6 ng/mL); this was also confirmed by stratifying patients according to age >70 years.” [13]
The p-value was 0.004, indicating high statistical significance; it is unlikely that this result from the study was caused by random chance. The PCR test looks for viral RNA in a swab sample from a patient. PCR-positive means that viral RNA from SARS-CoV-2, the Covid-19 virus, was found. Patients who are PCR-positive are presumed to have Covid-19, since they have the RNA from the virus that causes that disease. PCR-negative patients are presumed not to have Covid-19. Of course, both a positive or negative result could be mistaken. There were 107 total patients, with 27 who tested positive for Covid-19.
Patients with a positive test for Covid-19 had, on average, lower vitamin D levels than those who tested negative. This difference could be caused by vitamin D somehow making people less likely to become infected, such as by strengthening the immune system. But the correlation between low vitamin D levels and a positive test for Covid-19 is not conclusive. There could be other explanations. Correlation is not causation.
However, given the results of several other studies (including the six mentioned in part one of this article series), the evidence is building toward a conclusion that vitamin D has a protective effect against Covid-19. The means by which this protective effect is attained is not clear. But the information is still useful. It appears more and more likely that a population with higher blood levels of vitamin D will have a lower rate of infection, of severity, and of mortality regarding Covid-19.
9. Laird
This study compared infection rates as well as death rates for Covid-19 as compared to national average vitamin D levels [14]. They found that lower levels of vitamin D had a statistically significant correlation with higher mortality rates from Covid-19. They recommended optimizing vitamin D levels, as this will certainly have health benefits more generally, and may well help the population against Covid-19.
“Optimising vitamin D status to recommendations by national and international public health agencies will certainly have benefits for bone health and potential benefits for Covid-19. There is a strong plausible biological hypothesis and evolving epidemiological data supporting a role for vitamin D in Covid-19.” [14]
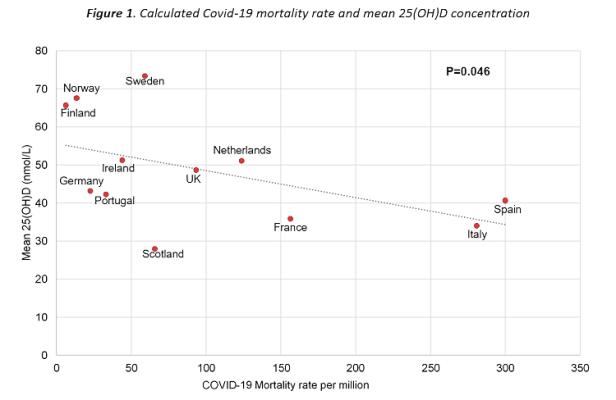
The p-value was 0.046, indicating statistical significance. The death rate for Covid-19 is inversely related to the blood levels of vitamin D in the population. Higher vitamin D levels indicate lower death rate from Covid. Vitamin D deficiency is correlated with higher death rates. And as the chart shows, there appears to be a stronger correlation between vitamin D deficiency and a high death rate than with high vitamin D levels and a lower death rate. Thus, a low level of vitamin D is more often associated with death than a high level is associated with survival. In other words, having a high level of vitamin D is often not enough to protect you from Covid-19. But having a low level of vitamin D is very often enough to make the disease much worse.
“In this short report we observed that low 25(OH)D concentrations appear to be associated with increased mortality from Covid-19. Countries with a formal vitamin D fortification policy appear to have the lowest rates of infection whilst countries with no policy and highest deficiency rates appear to be more adversely affected. This difference in Covid- 19 mortality by country has also been observed to form a North-South latitude gradient. Observational reports have also highlighted that Covid-19 infection and death rates appear to be higher in ethnic minority populations with darker skin which research has shown to be at much higher risk of vitamin D deficiency.” [14]
Other studies have also noted that darker skin, irrespective of race or ethnicity, is related to lower vitamin D and higher risk form Covid-19. The likely reason is that darker skin produces less vitamin D from exposure to sunlight than does lighter skin. Another factor is social and religious custom, which requires women to cover their skin, especially when outdoors. This results in lower vitamin D levels, and in higher risk from Covid-19. The solution to both issues, skin color and women who cover themselves, is to encourage vitamin D supplementation.
10. Faul
ARDS is Acute Respiratory Distress Syndrome. Severe cases of Covid-19 often include this syndrome. The discussion in the news media of the need for ventilators for Covid-19 patients is due to ARDS. Patients with this disorder cannot breathe on their own, not to a sufficient extent to obtain the oxygen they need. This study, published in the Irish Medical Journal, found that Covid-19 patients with low vitamin D had a greater risk of progressing to ARDS and a greater risk of requiring intubation and mechanical ventilation.
The study looked at 33 patients, all with Covid-19 and all requiring admission to the hospital. In this group, “twelve progressed to ARDS and required intubation and mechanical ventilation.” [15] These 12 had an average blood level of vitamin D (“serum 25OHD level”) of only 27 nmol/l (which is about 10.8 ng/ml). They were all clearly in a state of vitamin D deficiency. The other 21 patients, who did not develop ARDS nor need ventilation, had a higher blood level of vitamin D of 41 nmol/l (about 16.4 ng/ml). The difference was statistically significant.
Note that the patients who did not need ventilation and did not develop ARDS still had pneumonia and needed hospitalization. And when we compare their vitamin D levels to what is considered a normal or healthy level, they were below normal. So we might also conclude from this study (although the data was not analyzed this way), that low levels of vitamin D also increase risk of pneumonia and hospitalization, while very low levels increase risk of ARDS and ventilation.
Alipio versus Laird
Patients with normal vitamin D levels had only a 3.6% risk of a severe or critical case of Covid-19. “the odds of having a mild clinical outcome rather than a severe outcome were approximately 7.94 times (OR=0.126, p<0.001) while interestingly, the odds of having a mild clinical outcome rather than a critical outcome were approximately 19.61 times" [1] This agrees with one of the conclusions from the Laird study (#9 above), that having a high level of vitamin D only provides limited protection from Covid-19. But having a low level of vitamin D is enough to ensure that the disease will be much worse.
By way of analogy: suppose that you buy a very secure lock for the doors of your house. That may reduce burglaries. But they could also get into the house by the windows. So the amount of protection is limited. You need strong locks on the doors, but you need other protections as well. On the other hand, if you leave the front door unlocked, the increase in risk of burglary is much greater than the decrease in risk from a locked door. Similarly, low vitamin D greatly increases risk of a severe case of Covid-19, and even of death. But high vitamin D only provides a certain degree of protection. That degree of protection is substantial, and well worth the small cost and effort of taking a vitamin D supplement. But other factors also play into whether or not you become sick with Covid-19.
11. Meltzer
A new study found that untreated vitamin D deficiency was associated with a 77% increase in likelihood of Covid-19 infection. Persons with sufficient vitamin D were 56% less likely to become infected with Covid-19 [16]. There were 127 patients with vitamin D deficiency, and 291 with sufficient vitamin D. This is a relatively modest population side for a study, but enough for statistical significance.
The importance of this study is that, along with few others, at the top of this second article on vitamin D, it establishes a way to reduce likelihood of infection. In other words, vitamin D seems to have a preventative effect. The extent of this effect is limited and partial, but still useful. So vitamin D reduces chance of infection with Covid-19, reduces the severity of the disease, if you become infected, and reduces likelihood of death. That is a tremendous benefit from a simple safe vitamin.
12. Li
This study categorized U.S. States by latitude, and looked for a difference in case incidence and mortality for Covid-19.
“When the states were classified into high latitude (>N 37 degrees) and low latitude (<N 37 degrees) groups, both the cases (702 vs 255 cases/100k population) and deaths (43 vs 11 deaths/100k population) were significantly different (p < 0.001) between the two categories." [17]
At high latitudes (above 37 degrees), except in summer, the skin makes little vitamin D from exposure to UV light. At low latitudes, i.e. closer to the equator, there is much more vitamin D from exposure to the sun throughout much of the year. This difference gives persons living at low latitudes more vitamin D, and more of it throughout the year. If vitamin D affects Covid infection or mortality rates, there should be a difference between high and low latitude States for this reason. And there was. The study found a highly statistically significant difference in both case rate and death rate. This suggests that vitamin D reduces both the chances of becoming sick with Covid-19 and the chances of dying from that disease.
13. Pugach
In analysis of vitamin D data from 10 European nations, severe deficiency was strongly correlated with death from Covid-19 per million of the population [18].
14. Merzon
Merzon, Eugene, et al. “Low plasma 25(OH) vitamin D3 level is associated with increased risk of COVID-19 infection: an Israeli population-based study.” medRxiv (2020). — Low vitamin D increased risk (adjusted OR) of infection with Covid-19 by 45% and of hospitalization for Covid by 95% [19].
15. Panagiotou
Panagiotou, Grigorios et al., “Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity: results of a local audit of practice.” medRxiv (2020).
Conclusion: “we found that patients requiring ITU admission [in the ICU] were more frequently vitamin D deficient than those managed on medical wards [on the floor], despite being significantly younger.”
16. Chang
Chang, Timothy S., et al. “Prior diagnoses and medications as risk factors for COVID-19 in a Los Angeles Health System.” medRxiv (2020).
Risk factors included vitamin D deficiency, which increased risk of COVID-19 diagnosis by 80% (OR 1.8 [1.4-2.2], p=5.7 x 10-6).
17. Maghbooli
In this study, Vitamin D sufficiency reduced clinical severity and inpatient mortality [22]. “Only 9·7% of patients older than 40 years who were vitamin D sufficient succumbed to the infection compared to 20% who had a circulating level of 25(OH)D< 30 ng/mL. [22]" The death rate in persons over 40 was only 9.7% for those with sufficient blood levels of vitamin D. For those over 40 with vitamin D deficiency or insufficiency, the death rate was 20%.
Summary
Part one considered six studies, mainly looking at severity of disease and mortality. Sufficient evidence is presented in those six studies to show a strong statistically significant relation between low vitamin D and both severity of disease and mortality:
Alipio found that low vitamin D increased risk of a severe case of Covid-19; normal vitamin D increased odds of a mild case [1]. Lau found that low vitamin D increased risk of admission to a hospital Intensive Care Unit [2]. Daneshkhah found that low vitamin D increases risk of a severe case of Covid-19 [3]. Davies concluded that low vitamin D increased risk of a severe case and of death [4]. De Smet concluded that low vitamin D increased risk of the need for hospitalization, indicating a more severe case of Covid-19 [8]. Raharusun concluded that low vitamin D increased risk of death from Covid-19. “Only 4.1% of cases with normal Vitamin D levels died” [9].
Then in part two, above, the next three studies (Ilie, D’Avolio, Laird) also found an association between low vitamin D and the risk of simply contracting Covid-19 [12, 13, 14] as did the 11th study (Meltzer). Then Ilie and Laird also found an association between low vitamin D and death from Covid [12, 14]. Faul found that low vitamin D increased risk of admission to a hospital ICU [15]. Finally, Li et al. found that vitamin D from exposure of skin to the sun reduces both the population case rate and fatality rate from Covid.
These studies all found a correlation, not causation. But that fact does not allow us to dismiss the results. The ordinary progression in research of this type is to find a correlation, confirm that correlation with multiple studies, and then exclude other explanations apart from a direct or indirect connection between the factor under study (in this case blood levels of vitamin D) and the disease.
With a total of 12 studies, we have reached the point now where sufficient evidence supports the use of vitamin D supplementation as a way to fight against Covid-19. Vitamin D is an essential nutrient with many health benefits. It is known to be important to the immune system. And it may very well provide a substantial degree of protection from Covid-19.
The third part of this series of articles will examine expert commentary on these studies.
Ronald L Conte Jr
Covid.us.org
Note: the author of this article is not a doctor, nurse, or healthcare provider.
Endnotes
These begin at #12 because this is a continuation of an earlier article on the same topic.
12. Ilie, Petre Cristian, Simina Stefanescu, and Lee Smith. “The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality.” Aging Clinical and Experimental Research (2020): 1.
13. D’Avolio, Antonio, et al. “25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2.” Nutrients 12.5 (2020): 1359.
14. Laird, E., et al. “Vitamin D and Inflammation: Potential Implications for Severity of Covid-19.” Ir Med J; Vol 113; No. 5; P81: 2020.
15. Faul, J.L., et al. “Vitamin D Deficiency and ARDS after SARS-CoV-2 Infection.” Ir Med J; Vol 113; No. 5; P84: 2020.
16. Meltzer, David O., et al. “Association of Vitamin D Deficiency and Treatment with COVID-19 Incidence.” medRxiv (2020).
17. Li, Yajia, et al. “Sunlight and vitamin D in the prevention of coronavirus disease (COVID-19) infection and mortality in the United States.” (2020).
18. Pugach, Isaac Z. and Pugach, Sofya “Strong Correlation Between Prevalence of Severe Vitamin D Deficiency and Population Mortality Rate from COVID-19 in Europe.” medRxiv (2020).
19. Merzon, Eugene, et al. “Low plasma 25(OH) vitamin D3 level is associated with increased risk of COVID-19 infection: an Israeli population-based study.” medRxiv (2020).
20. Panagiotou, Grigorios et al., “Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity: results of a local audit of practice.” medRxiv (2020).
21. Chang, Timothy S., et al. “Prior diagnoses and medications as risk factors for COVID-19 in a Los Angeles Health System.” medRxiv (2020).
22. Maghbooli, Zhila, et al. “Vitamin D Sufficiency Reduced Risk for Morbidity and Mortality in COVID-19 Patients.” Available at SSRN 3616008 (2020).