As reported by Al Jazeera, Concerns mount as Iran gripped by third major COVID-19 wave. Here is the graph of deaths showing this “third wave” of deaths.
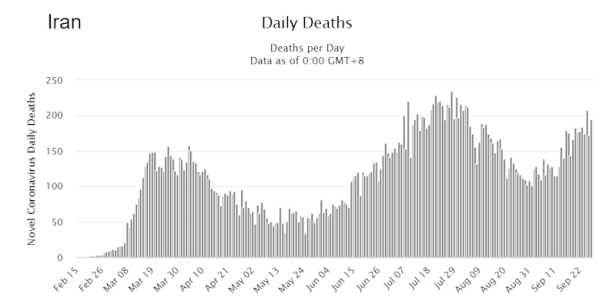
But between the “waves” there has hardly been any respite. Notice how the deaths per day remains fairly high, even between waves. Authorities have been diligent is promoting the usual precautions of wearing masks, social distancing, etc. But the disease continues unabated.
“In the past week, Supreme Leader Ayatollah Ali Khamenei and President Hassan Rouhani have issued direct warnings for people to better adhere to public health guidelines.”
“According to officials, Iran has joined COVAX, a global initiative aimed at working with vaccine manufacturers to provide countries equitable access to safe and effective vaccines once they are licensed and approved. Iran has also said it will buy 20 million doses of a vaccine made by an unnamed Indian company run by an Iran-born man.” [Al Jazeera]
According to Worldometers, Iran has had 449,960 reported cases and 25,779 reported deaths from Covid-19. With over 83 million persons, there is a great potential for increased harm from Covid-19 to the population. But if we look at the disease in many other nations, the severity varies greatly. Some nations now have low cases and lower deaths, and others are suffering greatly. What causes this difference?
Why is the Virus worse in Iran?
The main reason is likely vitamin D. Twenty-eight studies [1 - 28] show that low levels of vitamin D in the blood are associated with a higher risk of infection, higher risk of a severe case, and a higher risk of death from Covid-19. Vitamin D is produced in the human body when sunlight strikes skin. Populations with much exposure of sun to skin tend to have higher levels of vitamin D in the blood.
But Iran follows the customs of Islamic society, such that men and women keep their bodies covered, especially when outdoors in public. There is not much vitamin D from sunlight on skin, when little skin is exposed to the sun. Therefore, it is likely that even the healthiest persons in Iran have low vitamin D levels. This makes the population susceptible to Covid-19, a disease that is strongly affected by vitamin D.
Some nations, like Sweden, have a strong food fortification program, which requires food manufacturers to put vitamin D in various foods. This may be the reason that Sweden has not had a second wave of Covid-19 cases or deaths. But Iran does not have such a program. And not many foods have vitamin D in high amount naturally.
Then the only other way to obtain vitamin D is by a supplement, such as a pill or liquid or an injection (IM). This can be distributed quite easily to a population, as it is safe and effective to give a person 300,000 IU of vitamin D [29-31]. It also raises vitamin D levels quickly when a large “bolus” dose is given all at once. Another alternative is to give persons 10,000 IU per day, continuously throughout the pandemic. In either case, it can be expected that within 4 weeks the blood levels of vitamin D will have risen to the ideal level for lower risk of infection and very low risk of death from Covid-19.
Studies on Vitamin D
Twenty-eight studies, listed in the Endnotes as #1 - 28, show a correlation between vitamin D deficiency or vitamin D insufficiency and greater risk of Covid-19 infection and death. Having normal healthy blood levels of vitamin D reduces Covid-19 risks, including risk of infection [7, 8, 9, 11, 12, 14, 16, 23, 27], of having a severe case [1, 3, 4, 5, 15, 17, 20, 22, 24, 25, 26], of needing hospitalization, ICU care, and/or mechanical ventilation [2, 10, 14, 15, 21, 22, 24, 26], as well as the risk of dying from Covid-19 [4, 6, 7, 9, 12, 13, 17, 18, 19, 22, 24, 25, 28].
Some doctors have urged caution, and they point out the possibility of vitamin D toxicity or of higher blood calcium levels. But these risks are small compared to the great advantages that vitamin D offers in reducing the severity of the pandemic. And since it takes time for vitamin D levels in the blood to rise to good levels, after taking supplements as well as after getting out in the sun, we need to act as soon as possible.
Distribution of Vitamin D
Instead of having the population line up to receive a vaccine (and none is available yet), they could be given vitamin D in a massive national distribution program. It might be best to distribute the vitamin D in this manner. Selling supplements in stores can also work well, but there must be strict oversight to prevent unscrupulous persons from selling fake vitamin D pills. It would be difficult for anyone to know if they were getting the correct product and dosage. If the nation of Iran were to purchase vitamin D from India or China, the two major sources of supplements in the world, they could quickly distribute it, first to those that are at higher risk, government officials, health workers, etc., and soon after to the general population.
The only other way to raise vitamin D levels in the population in Iran is to have the government and religious authorities announce a temporary relaxation of restrictions on dress, so that people could expose skin to sunlight to make vitamin D. This is less expensive and easier for many persons; however, the amount of vitamin D produced is difficult to estimate. Health authorities should make an estimate of how much time to spend in the sun, depending on the time of day and how one is dressed. This might be done in the privacy of a balcony or enclosed yard. But it will be more difficult to do so modestly in the crowded urban conditions. So it will be left to authorities to decide the question.
For patients who already have Covid-19, vitamin D supplements take too long to go through the usual process in the body which changes vitamin D3 into its active form. One study [21] by Castillo, found that Covid-19 patients in hospital could be administered calcifediol, the form of vitamin D produced in the liver, shortening the time to activate the vitamin in the body. This produced a large decrease in the need for ICU care and therefore clearly a decrease in deaths for in-hospital patients.
The Solution to Iran’s Problem
The main solution is distribution of vitamin D to the population, in the form of one monthly dose of 300,000 IU of vitamin D or a daily dose of 10,000 IU. Vitamin D has been shown to reduce the risk of Covid-19 infection [7, 8, 9, 11, 12, 14, 16, 23]. One study found that persons with a vitamin D level in the middle of the normal range had half the risk of infection as compared to someone just above a level of deficiency (20 ng/ml; 50 nmol/l) [27]. But more importantly, vitamin D reduces risk of death from Covid-19 by as much as 90% [4, 6, 7, 9, 12, 13, 17, 18, 19, 22, 24, 25, 28]. In addition, other supplements and medications can be used to increase the effectiveness of the preventative measures (e.g. vitamin C, B vitamins, zinc, selenium). Then, for those who do become ill, the latest medications and interventions should be used.
Ronald L. Conte Jr.
Covid.us.org
Please note that I’m an author, not a doctor.
Endnotes:
1. Alipio, Mark. “Vitamin D Supplementation Could Possibly Improve Clinical Outcomes of Patients Infected with Coronavirus-2019 (COVID-19).” SSRN 3571484 (9 April 2020).
Study Link
2. Lau, Frank H., et al. “Vitamin D insufficiency is prevalent in severe COVID-19.” medRxiv (28 April 2020).
Study Link
3. Daneshkhah, Ali, et al. “The Possible Role of Vitamin D in Suppressing Cytokine Storm and Associated Mortality in COVID-19 Patients.” medRxiv (2020).
Study Link
4. Davies, Gareth, Attila R. Garami, and Joanna C. Byers. “Evidence Supports a Causal Model for Vitamin D in COVID-19 Outcomes.” medRxiv (2020).
Study Link
5. De Smet, Dieter, et al. “Vitamin D deficiency as risk factor for severe COVID-19: a convergence of two pandemics.” medRxiv (2020).
Study Link
6. Raharusun, Prabowo, et al. “Patterns of COVID-19 Mortality and Vitamin D: An Indonesian Study.” (2020).
PDF file
7. Ilie, Petre Cristian, Simina Stefanescu, and Lee Smith. “The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality.” Aging Clinical and Experimental Research (2020): 1.
Study Link
8. D’Avolio, Antonio, et al. “25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2.” Nutrients 12.5 (2020): 1359.
Study Link
9. Laird, E., et al. “Vitamin D and Inflammation: Potential Implications for Severity of Covid-19.” Ir Med J; Vol 113; No. 5; P81: 2020.
PDF file
10. Faul, J.L., et al. “Vitamin D Deficiency and ARDS after SARS-CoV-2 Infection.” Ir Med J; Vol 113; No. 5; P84: 2020.
PDF file
11. Meltzer, David O., et al. “Association of Vitamin D Deficiency and Treatment with COVID-19 Incidence.” medRxiv (2020).
Study Link
12. Li, Yajia, et al. “Sunlight and vitamin D in the prevention of coronavirus disease (COVID-19) infection and mortality in the United States.” (2020).
PDF file
13. Pugach, Isaac Z. and Pugach, Sofya “Strong Correlation Between Prevalence of Severe Vitamin D Deficiency and Population Mortality Rate from COVID-19 in Europe.” medRxiv (2020).
Study Link
14. Merzon, Eugene, et al. “Low plasma 25(OH) vitamin D3 level is associated with increased risk of COVID-19 infection: an Israeli population-based study.” medRxiv (2020). — Low vitamin D increased risk (adjusted OR) of infection with Covid-19 by 45% and of hospitalization for Covid by 95%.
Study Link
15. Panagiotou, Grigorios et al., “Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity: results of a local audit of practice.” medRxiv (2020). Conclusion: “we found that patients requiring ITU admission [in the ICU] were more frequently vitamin D deficient than those managed on medical wards [on the floor], despite being significantly younger.”
PDF file Link
16. Chang, Timothy S., et al. “Prior diagnoses and medications as risk factors for COVID-19 in a Los Angeles Health System.” medRxiv (2020).
Study Link
~ Risk factors included vitamin D deficiency, which increased risk of COVID-19 diagnosis by 80% (OR 1.8 [1.4-2.2], p=5.7 x 10-6).
17. Maghbooli, Zhila, et al. “Vitamin D Sufficiency Reduced Risk for Morbidity and Mortality in COVID-19 Patients.” Available at SSRN 3616008 (2020).
Study Link
~ Vitamin D sufficiency reduced clinical severity and inpatient mortality.
18. Panarese and Shahini, “Letter: Covid-19 and Vitamin D” Alimentary Pharmacology and Therapeutics, April 12, 2020.
Link to Letter
~ Covid-19 mortality increases with increasing latitude (by nation), and vitamin D blood levels decrease with increasing latitude. The authors propose that low levels of vitamin D increase Covid-19 mortality.
19. Carpagnano, Giovanna Elisiana, et al. “Vitamin D deficiency as a predictor of poor prognosis in patients with acute respiratory failure due to COVID-19.” Journal of Endocrinological Investigation (2020): 1-7. Study Link
~ “A survival analysis highlighted that, after 10 days of hospitalization, severe vitamin D deficiency patients had a 50% mortality probability, while those with vitamin D = 10 ng/mL had a 5% mortality risk (p = 0.019).”
20. Mardani, R., et al. “Association of vitamin D with the modulation of the disease severity in COVID-19.” Virus Research (2020): 198148. Study Link
21. Castillo, Marta Entrenas, et al. “Effect of Calcifediol Treatment and best Available Therapy versus best Available Therapy on Intensive Care Unit Admission and Mortality Among Patients Hospitalized for COVID-19: A Pilot Randomized Clinical study.” The Journal of Steroid Biochemistry and Molecular Biology (2020): 105751. Study Link
** This was a peer-reviewed randomized placebo-controlled trial (RCT). It’s sufficient. See the Chris Masterjohn, Ph.D. commentary here.
22. Radujkovic, et al. “Vitamin D Deficiency and Outcome of COVID-19 Patients.” Nutrients 2020, 12(9), 2757; Study Link
— “The present study demonstrates an association between VitD deficiency and severity of COVID-19.
VitD-deficient patients had a higher hospitalization rate and required more (intensive) oxygen therapy
and IMV. In our patients, when adjusted for age, gender, and comorbidities, VitD deficiency was
associated with a 6-fold higher hazard of severe course of disease and a ~15-fold higher risk of death.”
23. Israel, Ariel, et al. “The link between vitamin D deficiency and Covid-19 in a large population.” MedRxiv 9/7/2020. Study Link
24. Jae Hyoung Im, et al. “Nutritional status of patients with coronavirus disease 2019 (COVID-19).”
International Journal of Infectious Diseases. August 7, 2020. PDF Link
25. Gennari L, et al “Vitamin D deficiency is independently associated with COVID-19 severity and mortality” ASBMR 2020; Abstract 1023. Study Link
26. Baktash, Vadir, et al. “Vitamin D status and outcomes for hospitalised older patients with COVID-19.” Postgraduate Medical Journal (2020). Study Link
— “The main findings of our study suggest that older patients with lower serum concentrations of 25(OH)D, when compared with aged-matched vitamin D-replete patients, may demonstrate worse outcomes from COVID-19. Markers of cytokine release syndrome were raised in these patients and they were more likely to become hypoxic and require ventilatory support in HDU.” [HDU is high dependency unit]
27. Kaufman HW, et al. “SARS-CoV-2 positivity rates associated with circulating 25-hydroxyvitamin D levels.” (2020) PLoS ONE 15(9): e0239252. Study Link
— Optimum vitamin D blood level for reducing Covid-19 infection was found to be in the 50’s (ng/ml). This is the first study to show that 25(OH)D at levels above 30 have additional benefits.
28. Brenner, Hermann, Bernd Holleczek, and Ben Schöttker. “Vitamin D Insufficiency and Deficiency and Mortality from Respiratory Diseases in a Cohort of Older Adults: Potential for Limiting the Death Toll during and beyond the COVID-19 Pandemic?.” Nutrients 12.8 (2020): 2488.
— “Compared to those with sufficient vitamin D status, participants with vitamin D insufficiency and deficiency had strongly increased respiratory mortality, with adjusted hazard ratios (95% confidence intervals) of 2.1 (1.3–3.2) and 3.0 (1.8–5.2) overall, 4.3 (1.3–14.4) and 8.5 (2.4–30.1) among women, and 1.9 (1.1–3.2) and 2.3 (1.1–4.4) among men. Overall, 41% (95% confidence interval: 20–58%) of respiratory disease mortality was statistically attributable to vitamin D insufficiency or deficiency. Vitamin D insufficiency and deficiency are common and account for a large proportion of respiratory disease mortality in older adults, supporting the hypothesis that vitamin D3 supplementation could be helpful to limit the burden of the COVID-19 pandemic, particularly among women.”
29. Cesur, Yasar, et al. “Comparison of low and high dose of vitamin D treatment in nutritional vitamin D deficiency rickets.” Journal of pediatric endocrinology and metabolism 16.8 (2003): 1105-1110.
— In this study, infants and toddlers were given 150,000 IU, or 300,000 IU or 600,000 IU of vitamin D. The latter dose caused hypercalcemia, so the study authors recommended 150k or 300k IU of vitamin D (one time dose) for infants or toddlers to treat vitamin D deficiency.
30. Kearns, Malcolm, Jessica Alvarez, and Vin Tangpricha. “Large, single-dose, oral vitamin D supplementation in adult populations: a systematic review.” Endocrine Practice 20.4 (2014): 341-351.
— Recommended greater than or equal to 300,000 IU of vitamin D, but less than 500,000 IU, in a one-time dose to correct vitamin D deficiency.
31. Gupta, Nitin, et al. “Effect of oral versus intramuscular Vitamin D replacement in apparently healthy adults with Vitamin D deficiency.” Indian journal of endocrinology and metabolism 21.1 (2017): 131.
— Compared oral 60,000 IU weekly for 5 weeks to IM 300,000 IU one-time of vitamin D; both raised vitamin D levels just as well at 6 weeks; the latter dosing was better at 12 weeks.