I’ve been studying the research on Covid-19 since February, and I’ve read through hundreds of studies. I follow various physicians with YouTube channels specifically on Covid. And I’ve come to a conclusion: Covid-19 is seasonal. It is like the human coronaviruses that cause colds, in which the number of cases in winter is much higher than in summer. And this means that the number of Covid-19 cases in the U.S. in winter will be much higher than July. But July had nearly 2.0 million cases. Also, the death rate will be higher, not just as a higher number due to the higher case rate, but the percentage itself will also be higher.
Hypothetical example:
July, 2 million cases, death rate 1.35% = 27,000 deaths (actual number 26,703)
If the case rate increases by 50% in November:
Nov. 3 million cases…
death rate 1.35% — 40,500 deaths
death rate 4% — 120,000 deaths
death rate 6.6% — 198,000 deaths
So if the death rate states the same, but the number of cases goes up by 50%, then the number of deaths goes up by 50%. But if the death rate itself also increases, the number of cases is very much higher, as you can see in the above example.
By February, we could see a death rate of 6.6% or more, and a monthly number of cases several times the July rate of 2 million. As a result, monthly deaths could be as high as 0.5 to 1.0 million deaths in the U.S. alone in February alone. The worse months for seasonal illnesses tend to be Jan., Feb., March. It’s difficult to say which of those three will be the peak.
What causes this increase? Vitamin D levels in the blood. People are outside more in summer. Sunshine on skin makes vitamin D in the blood.
A high intake of vitamin D reduces risk of stroke [28], multiple sclerosis [29], rheumatoid arthritis [30], type 2 diabetes [31], breast cancer [32], prostate cancer [33], colon cancer [34], and all-cause mortality [35].
And 18 studies [1-18] show that vitamin D reduces Covid-19 risk, specifically, the risks of: infection [7, 8, 9, 11, 12, 14, 16], a severe case [1, 3, 4, 5, 15, 17], hospitalization and/or ICU care and/or ventilation [2, 10, 14, 15], and death [4, 6, 7, 9, 12, 13, 17, 18].
Winter 2020-2021
The U.S. had just under 2.0 million cases this past July. If Covid-19 is seasonal, the cases per month this winter will be a multiple of 2 million. And the death rate will not be the 1.35% of July, but more likely the 6.6% death rate of April. The number of deaths each month this winter could exceed 500,000 and could reach as high has 1 million. Those figures are total deaths per month, just in the U.S., against a case rate of several million to possibly over 10 or 15 million cases per month.
The U.S. healthcare system cannot handle that many cases. THE SYSTEM WILL BREAK. And then the death rate could go as high as 10, 15, or 20% of total cases. A typical death rate for hospitalized cases is 24%. Some of the better hospitals, those using the MATH+ Protocol, have death rates from 3.3% to 6.1% for hospitalized cases (that’s low!). But if the system breaks, many people will receive no care at all. If they can’t breathe, they will suffocate to death in their own homes, as there won’t be hospital equipment, beds, staff to treat them.
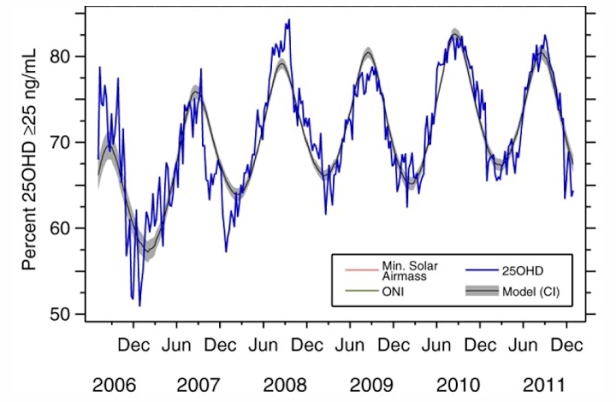
The SECOND WAVE is coming. The research proves it. Covid-19 is a vitamin D responsive illness. But vitamin D levels are much lower in winter than in spring:
We can AVERT the Second Wave with a massive vitamin D “supplementation and sunshine program”. It takes a month of high-dose vitamin D supplementation to raise vitamin D blood levels to the required point (over 40 ng/ml which is over 100 nmol/L).
We also need to do what Turkey did — build large 1,000 plus bed hospitals in 45 days: News.Sky.com and MiddleEastEye.com. Wikipedia: Dr. Oz Hospital and Dr. Murat Hospital.
The problem, of course, is that the U.S. does not have enough hospital beds. According to Statistica, the U.S. had 924,107 hospital beds in 2018. But hospitals typically run very close to capacity. It is not economical to maintain enough “beds” for a large surge of patients. By the way, the term “hospital beds” does not only mean physical beds, but the equipment and staff needed to serve the patients in those beds. So a pandemic can easily overwhelm the hospital system.
The Second Wave could seed 5 to 10 to 15 million new cases of Covid-19 per month this winter. The system cannot handle that many patients. Now 80% of those patients are mild or moderate, patients who might be treated at home. But 20% of 5 million is 1 million hospitalized Covid-19 patients, and we don’t have the beds. Even if we kick out of the hospital all other patients, we don’t have a million beds. Then at 10 or 15 million cases, the hospitalized number is 2 to 3 million in-patients. That’s two to three times the total number of hospital beds.
We should be building hospitals as Turkey did in under 60 days. But that’s only 1,000 beds per hospital. You just can’t build 1 to 3 thousand new hospitals — even if we had the money and the construction equipment, you couldn’t find enough hospital equipment to equip those new hospitals, and we don’t have enough doctors and nurses.
So the ONLY approach that will work is prevention. And there are few proven means to prevent Covid-19 or to prevent a severe case of Covid-19 or to prevent death from Covid-19. The most proven method is vitamin D supplementation. There is a study on hydroxychloroquine as a prophylactic [19]. Ivermectin was used as a prophylactic against scabies, and they inadvertently discovered that it worked against Covid-19 as a prophylactic as well [20]. Some persons take quercetin and zinc as a prophylactic, but there’s no clinical studies supporting that use. So vitamin D is our best prophylactic, at this point in time.
Now the FDA will tell you that vitamin D and other supplements or medications are not formally proven to prevent Covid-19 nor to decrease risk of a severe case or risk of death from Covid-19. But you go to war with the information you have, not the information you wish you had.
Children, 1-3: 2,000 IU/day
Children, 4-8: 3,000 IU/day
Children, 9-13: 4,000 IU/day
Teens, 14-18: 4,000 IU/day
Adults, 19-59: 10,000 IU/day
Seniors, 60+: 20,000 IU/day
Endnotes:
1. Alipio, Mark. “Vitamin D Supplementation Could Possibly Improve Clinical Outcomes of Patients Infected with Coronavirus-2019 (COVID-19).” SSRN 3571484 (9 April 2020).
Study Link
2. Lau, Frank H., et al. “Vitamin D insufficiency is prevalent in severe COVID-19.” medRxiv (28 April 2020).
Study Link
3. Daneshkhah, Ali, et al. “The Possible Role of Vitamin D in Suppressing Cytokine Storm and Associated Mortality in COVID-19 Patients.” medRxiv (2020).
Study Link
4. Davies, Gareth, Attila R. Garami, and Joanna C. Byers. “Evidence Supports a Causal Model for Vitamin D in COVID-19 Outcomes.” medRxiv (2020).
Study Link
5. De Smet, Dieter, et al. “Vitamin D deficiency as risk factor for severe COVID-19: a convergence of two pandemics.” medRxiv (2020).
Study Link
6. Raharusun, Prabowo, et al. “Patterns of COVID-19 Mortality and Vitamin D: An Indonesian Study.” (2020).
PDF file
7. Ilie, Petre Cristian, Simina Stefanescu, and Lee Smith. “The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality.” Aging Clinical and Experimental Research (2020): 1.
Study Link
8. D’Avolio, Antonio, et al. “25-hydroxyvitamin D concentrations are lower in patients with positive PCR for SARS-CoV-2.” Nutrients 12.5 (2020): 1359.
Study Link
9. Laird, E., et al. “Vitamin D and Inflammation: Potential Implications for Severity of Covid-19.” Ir Med J; Vol 113; No. 5; P81: 2020.
PDF file
10. Faul, J.L., et al. “Vitamin D Deficiency and ARDS after SARS-CoV-2 Infection.” Ir Med J; Vol 113; No. 5; P84: 2020.
PDF file
11. Meltzer, David O., et al. “Association of Vitamin D Deficiency and Treatment with COVID-19 Incidence.” medRxiv (2020).
Study Link
12. Li, Yajia, et al. “Sunlight and vitamin D in the prevention of coronavirus disease (COVID-19) infection and mortality in the United States.” (2020).
PDF file
13. Pugach, Isaac Z. and Pugach, Sofya “Strong Correlation Between Prevalence of Severe Vitamin D Deficiency and Population Mortality Rate from COVID-19 in Europe.” medRxiv (2020).
Study Link
14. Merzon, Eugene, et al. “Low plasma 25(OH) vitamin D3 level is associated with increased risk of COVID-19 infection: an Israeli population-based study.” medRxiv (2020). — Low vitamin D increased risk (adjusted OR) of infection with Covid-19 by 45% and of hospitalization for Covid by 95%.
Study Link
15. Panagiotou, Grigorios et al., “Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalised with COVID-19 are associated with greater disease severity: results of a local audit of practice.” medRxiv (2020). Conclusion: “we found that patients requiring ITU admission [in the ICU] were more frequently vitamin D deficient than those managed on medical wards [on the floor], despite being significantly younger.”
PDF file Link
16. Chang, Timothy S., et al. “Prior diagnoses and medications as risk factors for COVID-19 in a Los Angeles Health System.” medRxiv (2020).
Study Link
~ Risk factors included vitamin D deficiency, which increased risk of COVID-19 diagnosis by 80% (OR 1.8 [1.4-2.2], p=5.7 x 10-6).
17. Maghbooli, Zhila, et al. “Vitamin D Sufficiency Reduced Risk for Morbidity and Mortality in COVID-19 Patients.” Available at SSRN 3616008 (2020).
Study Link
~ Vitamin D sufficiency reduced clinical severity and inpatient mortality.
18. Panarese and Shahini, “Letter: Covid-19 and Vitamin D” Alimentary Pharmacology and Therapeutics, April 12, 2020.
Link to Letter
~ Covid-19 mortality increases with increasing latitude (by nation), and vitamin D blood levels decrease with increasing latitude. The authors propose that low levels of vitamin D increase Covid-19 mortality.
19. Kadnur, Harshith B., et al. “Hydroxychloroquine Pre-Exposure Prophylaxis for COVID-19 Among Healthcare Workers: Initial Experience from India.” (2020).
20. Valley View Nursing Home in Tornoto, Canada; Case series descried by Dr. Jennifer Hibberd
…
28. Marniemi et al., Dietary and serum vitamins and minerals as predictors of myocardial infarction and stroke in elderly subjects; Nutrition, Metabolism & Cardiovascular Diseases. Volume 15, Issue 3 , Pages 188-197, June 2005. Study Link
29. Munger et al., Vitamin D intake and incidence of multiple sclerosis; Neurology. January 13, 2004 vol. 62 no. 1, p. 60-65. Study Link
30. Merlino et al., Vitamin D intake is inversely associated with rheumatoid arthritis: Results from the Iowa Women’s Health Study; Arthritis & Rheumatism. Volume 50, Issue 1, pages 72-77, January 2004. Study Link
31. Pittas et al., Vitamin D and Calcium Intake in Relation to Type 2 Diabetes in Women; Diabetes Care. March 2006 vol. 29 no. 3 650-656. Study Link
32. Garland et al., Vitamin D and prevention of breast cancer: Pooled analysis; The Journal of Steroid Biochemistry and Molecular Biology, Volume 103, Issues 3-5, March 2007, Pages 708-711; Study Link
33. Garland et al., The Role of Vitamin D in Cancer Prevention; American Journal of Public Health. 2006 February; 96(2): 252-261. Study Link
34. Gorham et al., Optimal Vitamin D Status for Colorectal Cancer Prevention: A Quantitative Meta-Analysis; American Journal of Preventive Medicine. Volume 32, Issue 3 , Pages 210-216, March 2007; Study Link
35. Garland et al., The Role of Vitamin D in Cancer Prevention; American Journal of Public Health. 2006 February; 96(2): 252-261. Study Link